December 7, 2023
You might have heard of the concerns around antimicrobial resistance, whereby our antibiotics are becoming less effective, but did you know that HIV drug resistance is also a growing threat? According to the World Health Organization (WHO), up to 10% of adults starting HIV treatment have some level of drug resistance (meaning the virus had already mutated to become drug resistant when it was passed on to them).
The Public Health Agency of Canada’s National Microbiology Laboratory (NML) is a global leader in HIV drug resistance monitoring. The scientists at the NML, led by Dr. Hezhao Ji, Head of the Viral Genetics Unit, are working to expand international capacity to test for HIV drug resistance and innovate new, more precise testing methods to help protect the health of people in Canada and around the world.

Dr. Hezhao Ji, Head of the Viral Genetics Unit at NML
What is HIV drug resistance?
Over the years, advances in treating HIV using effective antiretroviral medicines have transformed HIV from a once fatal condition into a manageable chronic condition, where someone can live a long and healthy life. Antiretroviral medicine works by suppressing the levels of the virus in the body down to an undetectable level (learn more about Undetectable = Untransmittable). However, drug resistance can emerge with the increased use of these medicines.
In certain circumstances, for example, if the medication is not taken regularly or as prescribed, the virus can rebound and start to replicate again. When the virus replicates its genetic material, errors can occur, and some of those mistakes result in mutations. The mutated virus can become dominant and evade the antiretroviral medication, especially when the drugs present in the body are below the level needed to suppress the virus. Among patients where treatment no longer suppresses the virus, the prevalence of drug resistance to commonly used HIV medicines can range from 50% to 97%. While HIV drug resistance is the primary factor leading to treatment failure, other contributing factors include poor adherence while taking medications, inadequate dosing resulting from poor adherence or inaccurate prescription and individual variations among patients. HIV drug resistance and the treatment failure it causes can have serious consequences, causing HIV-related illness and death. It also means the virus can be passed on more easily leading to increased HIV transmission.
Global lab network monitors for HIV drug resistance
HIV drug resistance is monitored through genotypic testing, which can determine whether the known drug resistance mutations are present and then predict if the medicines will work effectively. The NML is part of the WHO global HIV drug resistance laboratory network, which consists of 34 WHO-designated laboratories that monitor for HIV drug resistance in different regions of the world. The NML was the first North American lab designated by the WHO in 2007. It stands as one of six specialized laboratories within this network (Canada has two, and is the only country with more than one specialized lab), undertaking some essential functions such as operational research, technical training and sample testing for countries that don’t have the capacity.
The NML actively contributes to global efforts against HIV drug resistance by developing new test guidelines, helping build lab capacity in other countries, and helping the WHO assess other laboratories seeking membership in the global network.
New technologies for more accurate HIV drug resistance testing
Dr. Ji is an internationally recognized expert in this field and has made significant contributions to the global effort in combating HIV drug resistance. Serving as the head of the HIV drug resistance program in the NML and as a member of two working groups under the WHO HIV Drug Resistance Network, his research focuses on developing new techniques to make testing for HIV drug resistance more cost efficient, timely and accurate.
“It’s rewarding to see our research make an impact in this field,” says Dr. Ji. “As a scientist, I want to use my expertise to improve people’s lives. That’s the most meaningful part for me in doing this work.”
The traditional HIV drug resistance testing methods detect drug resistant mutations in the samples at rates of 20% and above. Dr. Ji and his team developed a technique that can detect drug resistant variants present at as low as 1% by using a newer technology called next generation sequencing. This kind of sensitivity is important because such variants may only be present in a person’s body at 1% in the absence of drugs, but they may outgrow and become dominant when ineffective medication is used, resulting in treatment failure. This increased sensitivity in detecting low levels of drug resistant HIV variants can help health care providers to choose the most effective drugs for suppressing the virus in patients.
The NML is spearheading an international initiative to standardize next generation sequencing-based HIV genotyping technology for more widespread adoption. In pursuit of this goal, the NML hosted two international symposia in 2018 and 2019, bringing together leading experts from around the world with the aim of establishing operational guidelines for this advanced method. From the 2018 symposium, a comprehensive guideline for analyzing data from such testing was formulated, now known as the “Winnipeg consensus.”
Dried blood spot technology improves access to testing
The preferred specimen for HIV drug resistance testing is plasma, the liquid portion of the blood. However, this is not always practical in resource-limited settings. Dried blood spots (DBS) are increasingly used as an alternative specimen type for testing. The first WHO guideline for HIV drug resistance testing using DBS specimens, published in 2007, were built upon the protocol initially developed in the NML. The simplicity of this collection method allows HIV drug resistance monitoring to be done more easily in low to middle income countries. It also helps to address health inequities here in Canada—especially for individuals in northern, remote and isolated communities without immediate access to testing facilities.
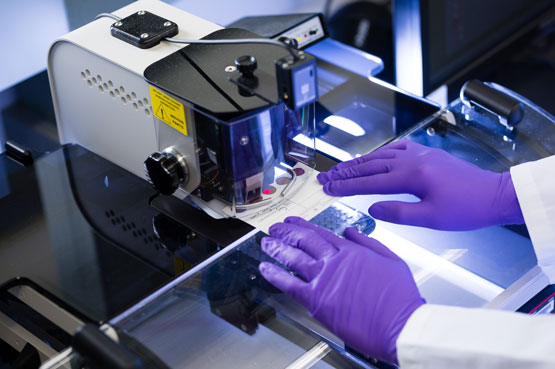
A scientist does dried blood spot testing.
Dr. Paul Sandstrom, Director of the NML’s Sexually Transmitted and Blood-Borne Infections Laboratories, cites the HIV drug resistance program as one of the examples of how the NML has become an internationally recognized centre for HIV research excellence.

Dr. Paul Sandstrom, Director, Sexually Transmitted and Blood-Borne Infections Laboratories, NML
“I’m extremely proud of the role the NML has carved out in this space. We view it as part of our service to people in Canada and around the world,” says Dr. Sandstrom.
